Problems with clunky electronic health record workflows – and the inability to share patient information between clinics – are driving some physicians right out of healthcare. But some facilities have figured out how to make things work more smoothly.
![Electronic Health Records [EHR] / digital medical data, monitor health status, doctor, laptop](https://www.computerworld.com/wp-content/uploads/2024/03/medical_data_status_tracking_electronic_health_records_ehr_by_metamorworks_gettyimages_1200x800-100760924-orig.jpg?quality=50&strip=all&w=1024)
FOXBORO, Mass. — While electronic healthcare records (EHRs) vastly improved patient information collection and sharing for some healthcare providers and payers, the technology also robs doctors of something critical: the ability to properly care for patients.
EHRs continue to require far too many mouse clicks and pagination to enter data during a visit, diverting attention from patients – something that’s key to not only creating a relationship but getting a complete picture of their health.
“Right now, it feels like physicians are a slave to their EHRs. There’s a high amount of burnout – emotional burnout, depersonalization and a low sense of professional accomplishment,” Dr. Alain Chaoui, former president of the Massachusetts Medical Society (MMS), said during a presentation last week at the New England HIMSS Annual Spring Conference here.
Between 50% and 70% of physicians are experiencing burnout symptoms due to EMR-related workloads, Chaoui said.
Chaoui, a practicing family physician who finished a one year stint as head of the MMS this month, said doctors are increasingly leaving healthcare through early retirement or moves to non-healthcare fields due to fatigue; others end up cutting back their patient hours to deal with the mundane administrative functions of healthcare.
For example, it can take as long as 45 minutes for a physician to schedule a CT scan for a patient via an EHR records system or over the telephone, with additional time spent cajoling an insurance provider to cover the procedure, Chaoui said.
“Today, doctors are on the computer all the time. EHRs were created for billing and not patient care,” Chaoui said. “Fixing EHRs at this point in time is urgent.”
EHRs – even those from the same vendor – are most often not interoperable between different healthcare facilities. It’s not uncommon, Chaoui said, for a patient’s radiology and blood work to be repeated each time they visit a different facility, even if it’s for the same issue, because the electronic records don’t share previous test results.
The problem is an old one. Some healthcare experts feel the issue has worsened due to regulatory changes in how facilities receive Medicare and Medicaid reimbursements. For example, those that were once reimbursed on the meaningful use of their EHRs must now attest as Accountable Care Organizations (ACOs) where quality measures are tied not only to patient care and costs, but the depth of data recorded in the records.
“That’s still an issue. Honestly, I don’t think we’ve gone too far,” said Jeff Loughlin, president-elect of New England HIMSS. “In some cases, it’s a little bit worse in the sense that you’ve got the onslaught of ACOs and quality contracts and things that require us to have individual data elements to do clinical quality measures that are now tied to performance.”
On the other hand, the needle on EHR interoperability has moved mainly through industry initiatives.
Loughlin pointed to the CommonWell Health Alliance and Carequality, nonprofit trade associations promoting vendor-neutral interoperability frameworks, including the Fast Healthcare Interoperability Resources (FHIR) standard, a set of APIs for exchanging EHR data. The Argonaut Project, another private sector effort to push for open interoperability standards – including FHIR – has also made significant headway, Loughlin said.
“We’re already seeing well over half of the EHRs adopting FHIR because they realize having a general consensus on a single platform makes sense for cost effectiveness and other applications,” Laughlin said. “We’ve made leaps forward, but the challenge moving forward … is that for a long time, every EHR was in their own little isolated world and it’s going to take time to break down those walls.”
Apple, for example, has based its mobile Health Records app on the FHIR specification and hospitals are adopting the technology to enable patients to control access to their own records.
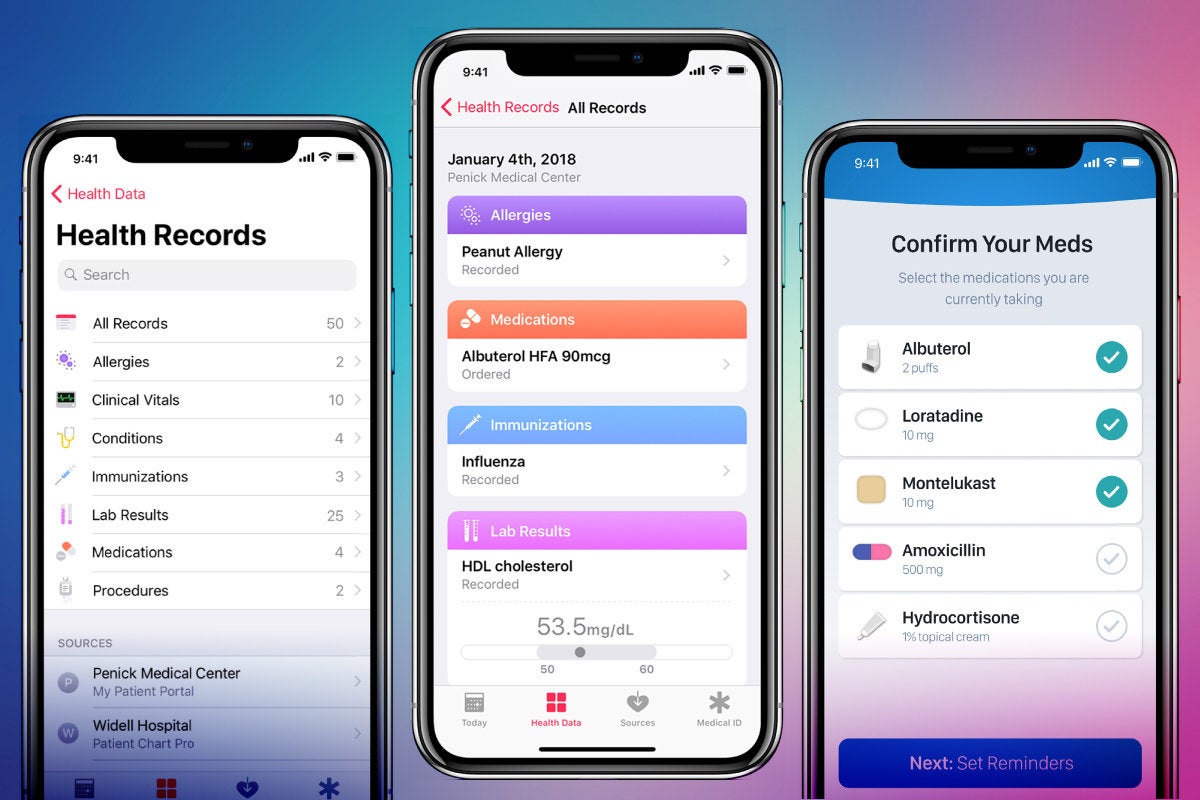 Apple
Apple
The UI for Apple’s Health Record app.
Judy Faulkner, CEO of Epic, whose EHR platform has the largest adoption rates, said in an interview earlier this year there’s no high correlation between physician burnout and satisfaction with EHR. In an interview in Healthcare IT News, Faulkner pointed to a recent study and clinician survey by KLAS Research showing dissatisfaction was more about a lack of training than actual software problems.
“If healthcare organizations offered higher-quality educational opportunities for their care providers – and if providers were expected to develop greater mastery of EHR functionality – many of the current EHR challenges would be ameliorated,” the study stated.
Falkner was unavailable for an interview on EHR usability and clinician burnout.
Dr. Larry Garber, director of clinical informatics for the Reliant Medical Group, said his organization has successfully reduced physician burnout but it wasn’t by allowing vendors to dictate functionality. The group practice in Worcester County, Mass. with 488 physicians throughout 43 locations first rolled out a homegrown EHR in 1993; it later used an Epic system deployed to allow more interoperability and smoother workflows.
The Reliant Medical Group’s ambulatory practice attained the Healthcare Information and Management Systems Society (HIMSS) analytics stage level 7 rating, which is a metric used to measure a healthcare facility’s ability to leverage EHRs and other technology to improve patient care.
Any EHR or health information exchange or any IT implementation needs to get three things right. First it needs to ensure that all healthcare stakeholders – from a hospital CFO to a physician to an administrative assistant – see value in the technology.
Second, it must efficiently fit into real-world workflows. Healthcare providers can’t be expected to surf multiple websites or click between multiple terminal screens to enter information while conducting a patient evaluation: click-counts matter. Patient data should be accessible on a single screen.
Third, trust is paramount. A patient needs to trust their data won’t be stolen; doctors and nurses should be confident an EHR is the best available and is implemented in the best way possible; and they need to know that when they identify a problem or have an idea, it will be considered or implemented.
“Our focus in terms of interoperability was we wanted to make sure whoever is taking care of our patients [that] they have all the information they need to do a better job taking care of them,” Garber said. “So we’ve done quite a bit of work on interoperability.”
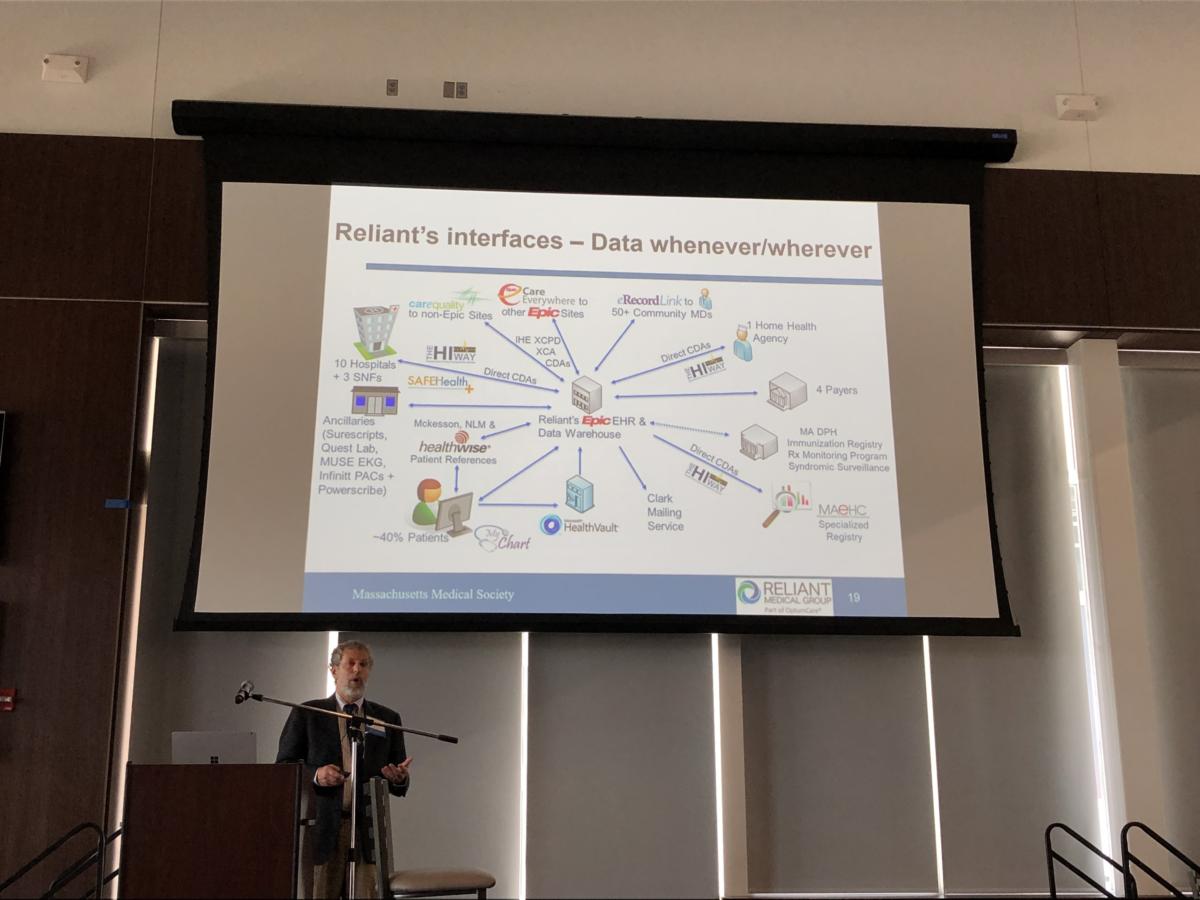 IDG/Reliant Medical Group
IDG/Reliant Medical Group
Dr. Larry Garber, director of clinical informatics for the Reliant Medical Group, illustrates on a slide the number of interfaces that have been created to share patient EHR data among clinics and improve workflows
The Reliant Medical Group has given 50 unassociated, regional physicians – who have treated the same patients as Reliant – access to its EHR system. They also enabled query access to its systems through Carequality.
Through Carequality, the medical group can see not only its own EPIC EHR system but Athena, eClinicalWorks and Cerner EHRs, among others.
“We’ve also set up a lot of point-to-point interfaces. We’re connected to 10 hospitals directly, so when my patients are in the hospital…, I get automatically sent to me…every single lab result, every single radiology report, procedure note,” Garber said. “All of those are loading directly into my EHR, so I don’t have to go look somewhere else to find these things.”
In addition, about 40% the group’s patients are active on its EHR web portal.
The EHR electronic “in-basket” is one of the biggest areas of complaints for doctors because others on a care team may not always be allowed to enter data; that leaves the doctor as the lone data entry clerk. The hospital group set up guidelines to enable nurses or other trusted healthcare providers to enter data as they’re speaking with a patient in person or over the telephone.
Another tweak the physician care group made to the EHR’s in-basket was to ensure lab results are properly marked. Typically, up to 50% of lab results can be marked as “abnormal,” but that doesn’t mean they require a physician’s attention.
“Sure, they’re abnormal technically, but they’re not really that abnormal,” Garber said. “So, we used decision support within our EHR to flag the things that are truly, significantly abnormal; these are critical…, these are things you have to pay attention to.”
“That helps reduce time invested looking at the EHR and it helps triage patients,” Garber added. “Consult notes, everything came to my in-basket. I don’t need to see most of those. So, we set it up where we automatically route important ones to me, and I don’t see the others. They’re in my EHR, I’ll see them the next time I see the patient.”
Automatic routing of critical lab results and consultation notes has reduced the amount of data in a physician’s in-basket by 25%, Garber said.
Massachusetts Medical Society’s Chaoui noted that while medical school graduates today may have been “born with a smart phone in their hand,” they enter the medical field frustrated at being tethered to an EHR desktop while attempting to evaluate patients.
“They don’t look at the patients anymore. We have created a new generation of fast users, but I don’t think this is what we’re looking for,” said Chaoui, who teaches a health informatics course at Northeastern University where he often hears medical student complaints about EHRs.
“Every time you’re in an exam room, every word counts and [the patient’s] body language counts,” Chaoui said. “We are losing this, and I’m begging you to bring this back to us.”








